Chapter 5
Tissues
5.2 Connective Tissue Supports and Protects
This section was edited and adapted from chapter 4.3 “The Tissue Level Organization: Connective Tissue Supports and Protects” of the open source book Anatomy and Physiology 2e from OpenStax (original text available for free at https://openstax.org/details/books/anatomy-and-physiology-2e).
Objectives
By the end of this section, you will be able to:
-
Identify and distinguish between the types of connective tissue: proper, supportive, and fluid
-
Explain the functions of connective tissues
As may be obvious from its name, one of the major functions of connective tissue is to connect tissues and organs. Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in between, connective tissue cells are dispersed in a matrix. The matrix usually includes a large amount of extracellular material produced by the connective tissue cells that are embedded within it. The matrix plays a major role in the functioning of this tissue. The major component of the matrix is a ground substance often crisscrossed by protein fibers. This ground substance is usually a fluid, but it can also be mineralized and solid, as in bones. Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of amorphous ground substance, and protein fibers. The amount and structure of each component correlates with the function of the tissue, from the rigid ground substance in bones supporting the body to the inclusion of specialized cells; for example, a phagocytic cell that engulfs pathogens and also rids tissue of cellular debris.
Functions of Connective Tissues
Connective tissues perform many functions in the body, but most importantly, they support and connect other tissues; from the connective tissue sheath that surrounds muscle cells, to the tendons that attach muscles to bones, and to the skeleton that supports the positions of the body. Protection is another major function of connective tissue, in the form of fibrous capsules and bones that protect delicate organs and, of course, the skeletal system. Specialized cells in connective tissue defend the body from microorganisms that enter the body. Transport of fluid, nutrients, waste, and chemical messengers is ensured by specialized fluid connective tissues, such as blood and lymph. Adipose cells store surplus energy in the form of fat and contribute to the thermal insulation of the body.
Classification of Connective Tissues
There are three broad categories of connective tissue, connective tissue proper, supportive connective tissue, and fluid connective tissue. The classification is based on the characteristics of their ground substance and the types of fibers found within the matrix (Table 5.1).
| Connective tissue proper | Supportive connective tissue | Fluid connective tissue |
|---|---|---|
| Loose connective tissue | Cartilage | Blood |
| • Adipose | • Hyaline | |
| • Areolar | • Fibrocartilage | |
| • Reticular | • Elastic | |
| Dense connective tissue | ||
| • Dense regular |
Connective Tissue Proper
Connective tissue proper includes loose connective tissue and dense connective tissue. Both tissues have a variety of cell types and protein fibers suspended in a viscous ground substance.
Cell types include fibroblasts, adipocytes or fat storage cells, and mesenchymal cells. Fibroblasts secrete fibers into the ground substance. Adipocytes store lipids. Brown adipocytes store lipids as many droplets, and have high metabolic activity. White adipocytes store lipids in one large drop and are metabolic less active. Mesenchymal cells are cells that can become any connective tissue cell.
The fibroblasts secret three main fibres: collagen, elastic, and reticular fibers (Table 5.2). Collagen fibers are made of fibrous proteins that form long and strait fibers. Collagen fibers, while flexible, have great tensile strength. Tensile strength is the force needed to pull a material to the point that it breaks. Elastic fibers contain the protein elastin. Elastin will return to its original shape after being stretched or compressed. Reticular fibers are short, fine collagenous fibers that form a network.
| Fiber | Purpose | Location |
|---|---|---|
| Collagen fibers | Bind bones and other tissue to each other | Tendon, ligament, skin, cornea, cartilage, bone, blood vessels, gut, intervertebral disc |
| Elastic fibers | Allow organs like arteries and lungs recoil | Extracellular matrix |
| Reticular fibers | Form a scaffolding for other cells | Liver, bone marrow, lymphatic organs |
In loose connective tissue, fibers are loosely organized, leaving large spaces in between. It is found between many organs where it acts both to absorb shock and binds tissues together. There are three types of loose connective tissue, adipose, areolar, and reticular tissue.
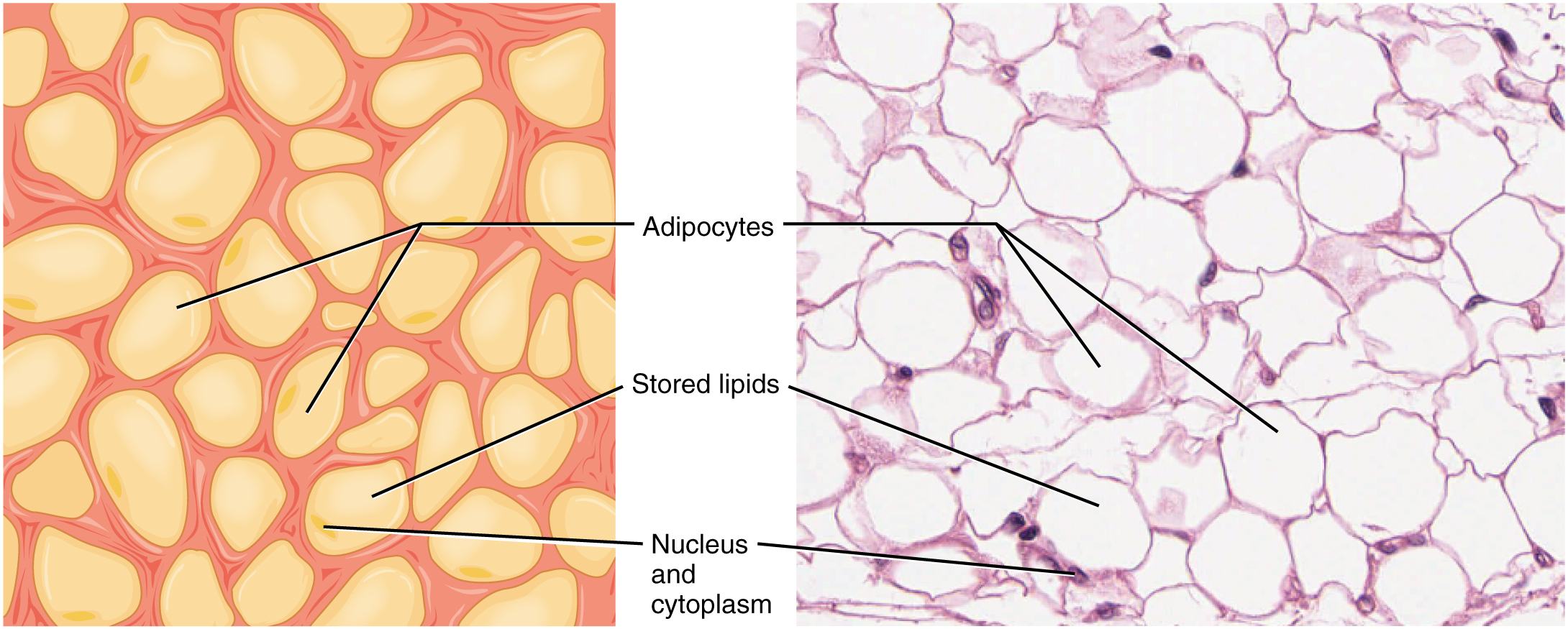
Adipose tissue consist mostly of fat storage cells (adipocytes), with little extracellular matrix (Figure 5.9). White adipose tissue is most abundant. It contributes mainly to lipid storage and can serve as insulation from cold temperature and mechanical injury. For example, it protects the kidneys and cushions the back of the eye. Brown adipose tissue is mainly found in infants, hence the term “baby fat”. In adults it is mainly found in the neck and shoulder (clavicular) region. Brown fat tissue has many mitochondria and is very efficient in metabolizing stored fat. In contrast to white fat, when brown fat is broken down metabolic heat is released and not adenosine triphoshate (ATP), a key molecule used in metabolism. Thus, brown fat is mainly used to maintain the body temperature. Areolar tissue contains all the cells and fibers previously described and is distributed in a random, web-like fashion. It fills the spaces between muscle fibers, surrounds blood and lymph vessels, and supports organs in the abdominal cavity. It underlies most epithelia and represents the connective tissue component of epithelial membranes. It is a reservoir of water and salts for surrounding tissues.
Reticular tissue is a mesh-like, supportive framework for soft organs such as lymphatic tissue, the spleen, and the liver (Figure 5.10). It derives its name from the Latin reticulus, which means “little net.”

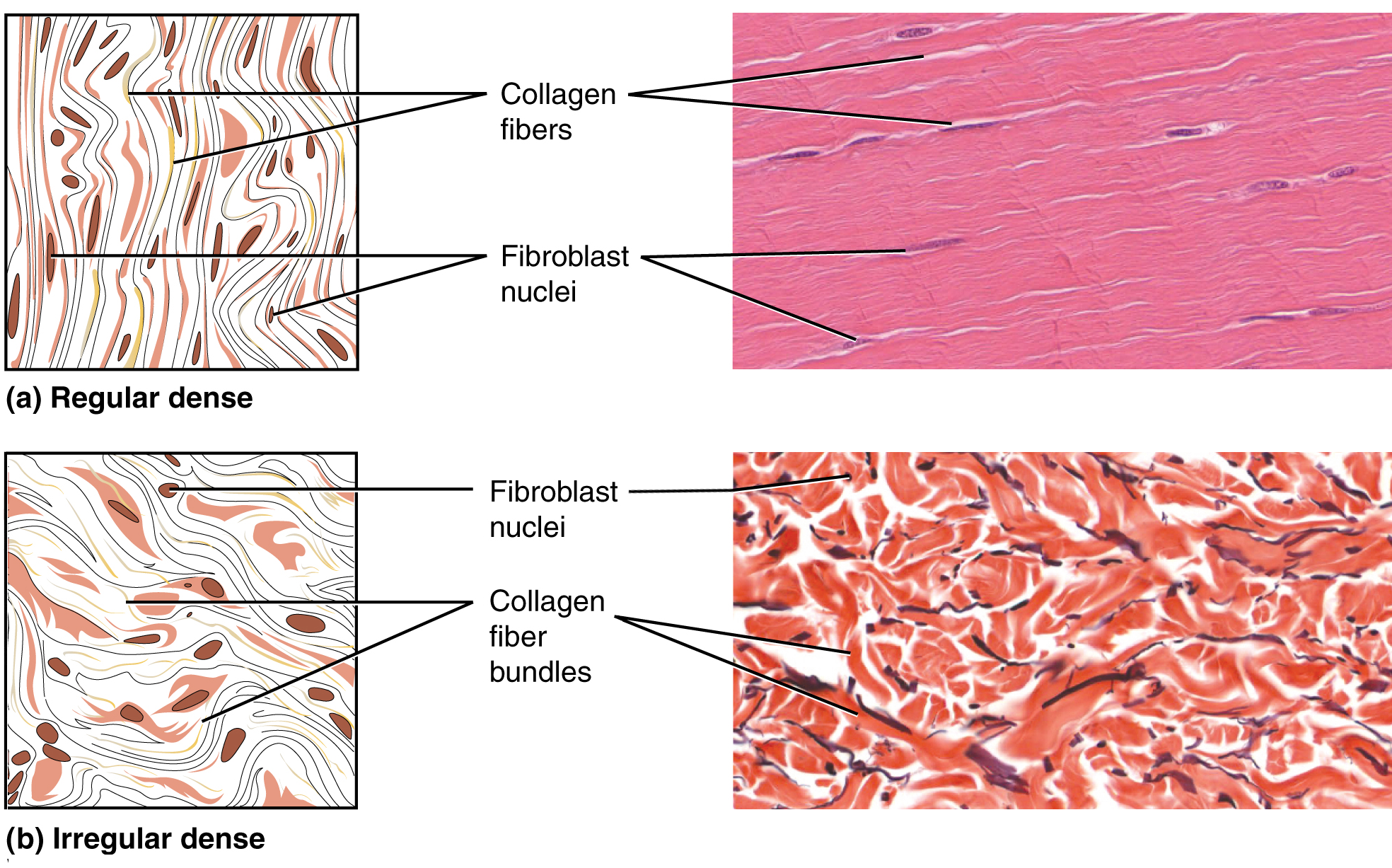
Dense connective tissue contains more collagen fibers than does loose connective tissue. As a consequence, it displays greater resistance to stretching. There are two major categories of dense connective tissue: regular and irregular (Table 5.1). In dense regular connective tissue fibers are parallel to each other, enhancing tensile strength and resistance to stretching in the direction of the fiber orientations. Ligaments and tendons are made of dense regular connective tissue, but in ligaments not all fibers are parallel. Dense regular elastic tissue contains elastin fibers in addition to collagen fibers, which allows the ligament to return to its original length after stretching. The ligaments in the vocal folds and between the vertebrae in the vertebral column are elastic. In dense irregular connective tissue, the direction of fibers is random. This arrangement gives the tissue greater strength in all directions and less strength in one particular direction. In some tissues, fibers crisscross and form a mesh. In other tissues, stretching in several directions is achieved by alternating layers where fibers run in the same orientation in each layer, and it is the layers themselves that are stacked at an angle. The dermis of the skin is an example of dense irregular connective tissue rich in collagen fibers. Dense irregular elastic tissues give arterial walls the strength and the ability to regain original shape after stretching (Figure 5.11).
Disorders of the Connective Tissue: Tendinitis
Your opponent stands ready as you prepare to hit the serve, but you are confident that you will smash the ball past your opponent. As you toss the ball high in the air, a burning pain shoots across your wrist and you drop the tennis racket. That dull ache in the wrist that you ignored through the summer is now an unbearable pain. The game is over for now.
After examining your swollen wrist, the doctor in the emergency room announces that you have developed wrist tendinitis. She recommends icing the tender area, taking non-steroidal anti-inflammatory medication to ease the pain and to reduce swelling, and complete rest for a few weeks. She interrupts your protests that you cannot stop playing. She issues a stern warning about the risk of aggravating the condition and the possibility of surgery. She consoles you by mentioning that well known tennis players such as Venus and Serena Williams and Rafael Nadal have also suffered from tendinitis related injuries.
What is tendinitis and how did it happen? Tendinitis is the inflammation of a tendon, the thick band of fibrous connective tissue that attaches a muscle to a bone. The condition causes pain and tenderness in the area around a joint. On rare occasions, a sudden serious injury will cause tendinitis. Most often, the condition results from repetitive motions over time that strain the tendons needed to perform the tasks.
Persons whose jobs and hobbies involve performing the same movements over and over again are often at the greatest risk of tendinitis. You hear of tennis and golfer’s elbow, jumper’s knee, and swimmer’s shoulder. In all cases, overuse of the joint causes a microtrauma that initiates the inflammatory response. Tendinitis is routinely diagnosed through a clinical examination. In case of severe pain, X-rays can be examined to rule out the possibility of a bone injury. Severe cases of tendinitis can even tear loose a tendon. Surgical repair of a tendon is painful. Connective tissue in the tendon does not have abundant blood supply and heals slowly.
While older adults are at risk for tendinitis because the elasticity of tendon tissue decreases with age, active people of all ages can develop tendinitis. Young athletes, dancers, and computer operators; anyone who performs the same movements constantly is at risk for tendinitis. Although repetitive motions are unavoidable in many activities and may lead to tendinitis, precautions can be taken that can lessen the probability of developing tendinitis. For active individuals, stretches before exercising and cross training or changing exercises are recommended. For the passionate athlete, it may be time to take some lessons to improve technique. All of the preventive measures aim to increase the strength of the tendon and decrease the stress put on it. With proper rest and managed care, you will be back on the court to hit that slice-spin serve over the net. Watch the YouTube video below to learn more about tendonitis.
Supportive Connective Tissues
Two major forms of supportive connective tissue, cartilage and bone, allow the body to maintain its posture and protect internal organs.
Cartilage has a distinctive appearance due to polysaccharides called chondroitin sulfates, which bind with ground substance proteins to form proteoglycans. Embedded within the cartilage matrix are chondrocytes, or cartilage cells, and the space they occupy are called lacunae (singular = lacuna). A layer of dense irregular connective tissue the perichondrium, encapsulates the cartilage. Cartilaginous tissue is avascular (i.e., without blood vessels), thus all nutrients need to diffuse through the matrix to reach the chondrocytes. This is a factor contributing to the very slow healing of cartilaginous tissues.
The three main types of cartilage tissue are hyaline cartilage, fibrocartilage, and elastic cartilage (Figure 5.12). Hyaline cartilage, the most common type of cartilage in the body, consists of short and dispersed collagen fibers and contains large amounts of proteoglycans. Under the microscope, tissue samples appear clear. The surface of hyaline cartilage is smooth. Both strong and flexible, it is found in the rib cage and nose and covers bones where they meet to form moveable joints. It makes up a template of the embryonic skeleton before bone formation. A plate of hyaline cartilage at the ends of bone allows continued growth until adulthood. Fibrocartilage is tough because it has thick bundles of collagen fibers dispersed through its matrix. Menisci (singular = meniscus) in the knee joint and the intervertebral discs are examples of fibrocartilage. Elastic cartilage contains elastic fibers as well as collagen and proteoglycans. This tissue gives rigid support as well as elasticity. Tug gently at your ear lobes, and notice that the lobes return to their initial shape. The external ear contains elastic cartilage.

Bone is the hardest connective tissue. It provides protection to internal organs and supports the body. Bone’s rigid extracellular matrix contains mostly collagen fibers embedded in a mineralized ground substance containing hydroxyapatite, a form of calcium phosphate. Both components of the matrix, organic and inorganic, contribute to the unusual properties of bone. Without collagen, bones would be brittle and shatter easily. Without mineral crystals, bones would flex and provide little support. Osteocytes, bone cells like chondrocytes, are located within lacunae. The histology of transverse tissue from long bone shows a typical arrangement of osteocytes in concentric circles around a central canal. The central canal contains nerves, lymphatic and blood vessels. Thus, bone is a highly vascularized tissue. Unlike cartilage, bone tissue can recover from injuries in a relatively short time.
There are two types of bone tissue, cancellous or spongy, and compact bone tissue. Most bones have both tissues. Spongy (cancellous) bones looks like a sponge under the microscope and contain spaces between so-called trabeculae (singular = trabecula) (or arches of bone proper). The spaces are often filled with red bone marrow. The trabeculae form a network and contain the osteocytes in lacunae. Spongy bone is lighter than compact bone. Compact bone has a greater structural strength. In compact bones the osteocytes are in lacunae within concentric rings of calcified matrix called lamellae (singular: lamella). (Figure 5.13).

Fluid Connective Tissue
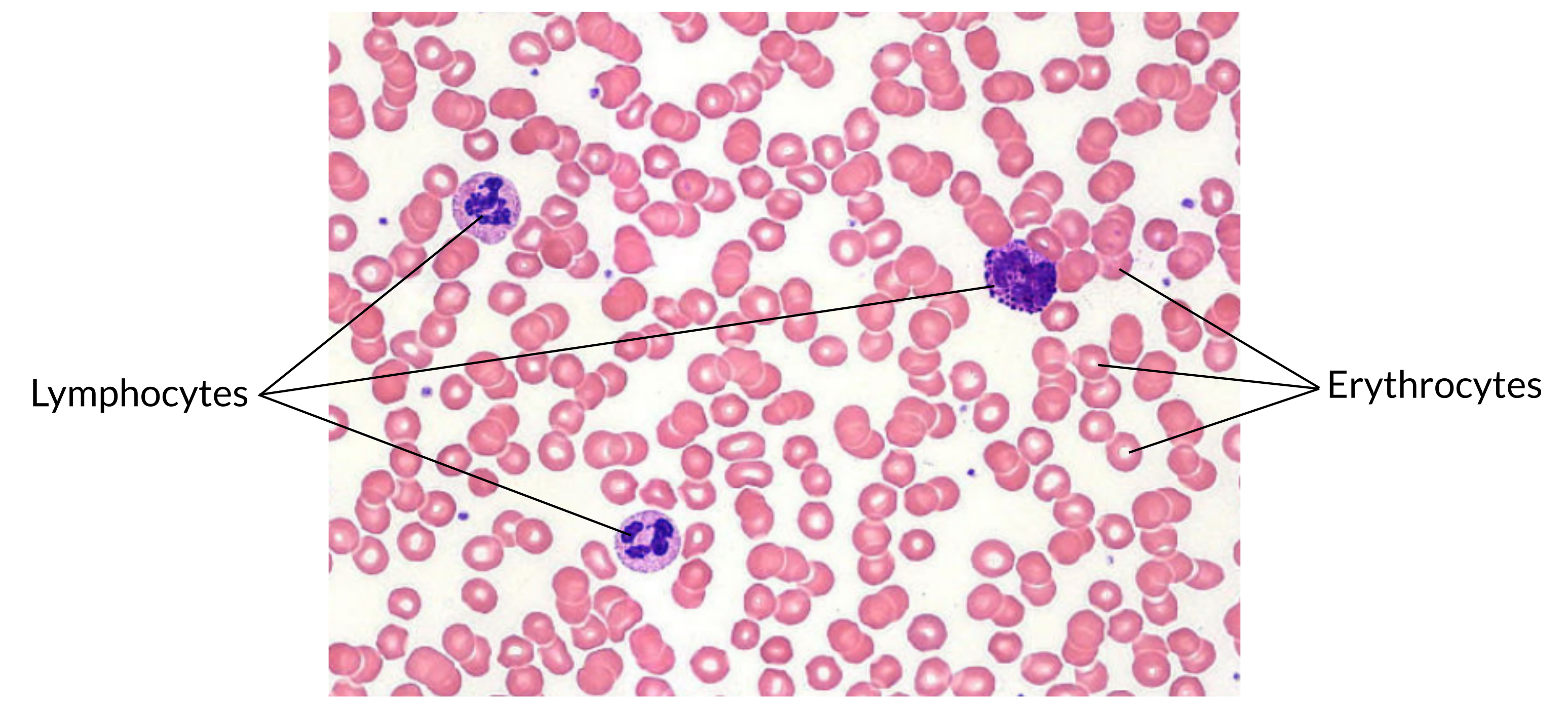
Blood and lymph are fluid connective tissues. Cells circulate in a liquid extracellular matrix (Figure 5.14). The formed elements circulating in blood are all derived from hematopoietic stem cells located in bone marrow. Erythrocytes, red blood cells, transport oxygen and some carbon dioxide. Leukocytes, white blood cells, are responsible for defending against potentially harmful microorganisms or molecules. Platelets are cell fragments involved in blood clotting. Some white blood cells have the ability to cross the endothelial layer that lines blood vessels and enter adjacent tissues. Nutrients, salts, and wastes are dissolved in the liquid matrix and transported through the body.
Lymph contains a liquid matrix and white blood cells. Lymphatic capillaries are extremely permeable, allowing larger molecules and excess fluid from interstitial spaces to enter the lymphatic vessels. Lymph drains into blood vessels, delivering molecules to the blood that could not otherwise directly enter the bloodstream. In this way, specialized lymphatic capillaries transport absorbed fats away from the intestine and deliver these molecules to the blood.
Key Terms
- adipose tissue
- specialized areolar tissue rich in stored fat
- areolar tissue
- a type of connective tissue proper that shows little specialization with cells dispersed in the matrix
- chondrocytes
- cells of the cartilage
- clotting
- also called coagulation; complex process by which blood components form a plug to stop bleeding
- collagen fiber
- flexible fibrous proteins that give connective tissue tensile strength
- connective tissue
- type of tissue that serves to hold in place, connect, and integrate the body’s organs and systems
- connective tissue proper
- connective tissue containing a viscous matrix, fibers and cells
- dense connective tissue
- connective tissue proper that contains many fibers that provide both elasticity and protection
- elastic cartilage
- type of cartilage, with elasitn as the major protein, characterized by rigid suppoer as well as elasticity
- elastic fiber
- fibrous protein within connective tissue that contains a high percentage of the protein elastin that allows the fiber to stretch and return to original size
- erythrocytes
- red blood cells
- fibroblast
- most abundant cell type in connective tissue, secretes protein fibers and matrix into the extracellular space
- fibrocartilage
- tough form of cartilage, made of thick bundles of collagen fibers embedded in chondroitin sulfate ground substance
- fluid connective tissue
- specialized cells that circulate in a watery fluid containing salts, nutrients, and dissolved proteins
- ground substance
- fluid or semi-fluid portion of the matrix
- hyaline cartilage
- most common type of cartilage, smooth and made of short collagen fibers embedded in chondroitin sulfate ground substance
- lacunae
- (singular = lacuna) small space in bone or cartilage tissue that cells occupy
- lamina propria
- areolar connective tissue underlying a mucous membrane
- leukocytes
- white blood cells
- loose connective tissue
- type of connective tissue proper that shows little specialization with cells dispersed in the matrix
- matrix
- extracellular material which is produced by the cells embedded in it, containing ground substance and fibers
- mesenchymal cell
- adult stem cell from which most connective tissue cells are derived
- osteocytes
- bone cells
- reticular fiber
- fine fibrous protein, made of collagen subunits, which cross-link to form supporting “nets” within connective tissue
- reticular tissue
- type of loose connective tissue that provides a supportive framework to soft organs, such as lymphatic tissue, spleen, and the liver
- supportive connective tissue
- type of connective tissue that provides strength to the body and protects soft tissue
Review Questions
- Question 5.2.1
-
- Question 5.2.2
-
- Question 5.2.3
-
- Question 5.2.4
-
- Question 5.2.5
-
- Question 5.2.6
-
